Why Does Psoriasis Recur?
October 21, 2018
Author: Admin Editor
Tags:
Psoriasis is a disease of the immune system in which inflammation causes skin cells to multiply faster than normal. They cause raised, red patches covered by silvery scales when they reach the surface of the skin and die. It occurs most commonly on the scalp, knees, elbows, hands, and feet, but can also appear on the lower back, face, genitals, nails, and other places. The American Academy of Dermatology estimates psoriasis affects about 7.5 million Americans.
Research at Brigham and Women's Hospital and Rockefeller University is helping to address a longstanding question about this inflammatory skin condition: Why do skin lesions that have resolved with therapy recur in the same locations after a patient stops using topical steroids?
Researchers have been searching for years for a cell population that continues to smolder after psoriasis appears to resolve. It's been challenging to zoom in on the population of T cells driving the disease in part because when psoriasis is active, lesions are flooded with diverse T cells.
BWH physician scientist Rachael Clark, MD, Ph.D. of the Department of Dermatology and her colleagues have taken a new approach. Instead of looking during the height of activity, they examined lesion sites after treatment. They identified T cell receptors of cells at these sites that were shared across psoriatic patients but not found in healthy individuals or those with other skin conditions.
The team's findings are reported in the Journal of Clinical Investigation. "When psoriasis is treated, T cells that flooded in during inflammation recede like the tide," Clark said. "They leave behind a population of cells that stand out."
The population of T cells that remains are tissue resident memory cells, which live long term in skin and, when functioning properly, should be fighting infection. But for patients with psoriasis, these cells may be the source of the misguided immune response that leads to red, inflamed patches on the skin.
To identify this T cell population, the researchers took biopsies at the sites of active lesions before treatment and biopsies of the same skin areas after the lesions had cleared on therapy. Using high-throughput sequencing and immunostaining, the research team found that resolved lesions contained populations of T cells derived from just a few cells - known as oligoclonal populations - that produced IL-17, a telltale marker of inflammation.
These cells also shared stretches of genetic sequence that code for the same antigen receptors. These shared T cell antigen receptors were found only among cells from psoriatic patients - not in cells from healthy controls or people with skin conditions such as atopic dermatitis.
This work highlights the fact that most psoriasis treatments do not kill these disease causing T cells but instead temporarily suppress their activation. Now that they have identified the long lived, skin resident T cell population that appears to be driving recurrence, the team plans to search for new therapies that can deplete these resident T cells, potentially driving the disease into long-term remission.
"We believe these resident memory T cells are the root of the problem, Clark added. Imagine these cells are teenagers throwing a party. They invite lots of other cells to the site of the party, making it hard to identify them while the party is in full swing. It's only after inflammation dies down and everyone else goes home that we can see these culprits. A small number of cells can cause so much trouble. But depleting this population of cells may be the key to slowing down this disease or preventing its recurrence."
Psoriasis Severity Linked To Increased Risk Of Type 2 Diabetes
People with psoriasis are also at a higher risk to develop type-2 diabetes than those without psoriasis, and the risk increases dramatically based on the severity of the disease. Researchers from the Perelman School of Medicine at the University of Pennsylvania found people with psoriasis that covers 10 percent of their body or more are 64 percent more likely to develop diabetes than those without psoriasis, independent of traditional risk factors such as body weight.
Applying the study's findings published in the Journal of the American Academy of Dermatology - to the number of people who have psoriasis worldwide would equate to 125,650 new cases of diabetes attributable to psoriasis per year.
The type of inflammation seen in psoriasis is known to promote insulin resistance, and psoriasis and diabetes share similar genetic mutations suggesting a biological basis for the connection between the two conditions we found in our study, says the study's senior author Joel M. Gelfand, MD MSCE, a professor of Dermatology and Epidemiology at Penn.
We know psoriasis is linked to higher rates of diabetes, but this is the first study to specifically examine how the severity of the disease affects a patients risk.
Understanding Additional Risks
In order to measure psoriasis severity, the researchers used body surface area (BSA), which measures the percentage of the body covered by psoriasis. Using a United Kingdom database, they surveyed general practitioners about BSA affected by psoriasis and looked at data on 8,124 adults with psoriasis and 76,599 adults without psoriasis over the course of four years. They adjusted the samples to account for any differences in age, sex, and body mass index and other diabetes risk factors.
They found patients with a BSA of two percent or less had a relative risk of 1.21 for developing diabetes, meaning their risk is 21 percent higher than those without psoriasis. This risk increased dramatically in patients with a BSA of 10 percent or more.
On average, 5.97 out of every 1,000 people will get diabetes in a given year. In the population of patients with a BSA greater than 10 percent, that number jumps to 12.22 per 1,000 people. That group had a relative risk of 1.64, or 64 percent higher than patients with no psoriasis at all.
Further, they found that for every 10 percent increase in BSA beyond the initial 10 percent, the relative risk increased by another 20 percent. In other words, patients with 20 percent BSA were at almost an 84 percent higher risk of developing type-2 diabetes, patients with 30 percent BSA were at a 104 percent higher risk, and so on.
These findings are independent of traditional risk factors for diabetes and still show a strong connection between the increasing severity of psoriasis and the increasing risk of developing diabetes, which makes a strong argument for a causal relationship between the two, Gelfand said.
He added that psoriasis BSA should be routinely measured, and patients targeted for diabetes prevention, especially in those with a BSA of 10 percent or higher. These results add to the growing understanding of the additional risks associated with severe psoriasis, which his other studies have shown can include major cardiovascular events, liver disease and death.
Link Between Severe Psoriasis And Increased Risk Of Death
The more the surface area of the body is covered by psoriasis, the greater the risk of death for the patient suffering from the condition, according to another study by the same researchers.
The study published in the Journal of Investigative Dermatology, is the first to link psoriasis severity to an increased risk of death using an objective measure of disease severity called Body Surface Area (BSA) rather than treatment patterns, such as whether or not a patient was receiving oral, injectable or phototherapy treatment for the condition. It finds patients with psoriasis on 10 percent or more of their body are at almost double the risk of death.
It's well established that psoriasis is associated with an increased risk for other comorbidities like chronic kidney disease, diabetes, and cardiovascular disease, but we dont yet understand how the severity of psoriasis impacts future risk of major health problems, Gelfand said.
For this study, Gelfand and his team again used the Body Surface Area metric. Using a database from the United Kingdom, they looked at 8,760 patients with psoriasis and 87,600 people without it. They sent surveys to the patients general practitioners to determine the body surface area affected by psoriasis as this information is not routinely available in medical records.
They then looked at the number of deaths in each group by person-years, a measure that combines the number of people with the amount of years of data on them in the database.
The team used an average follow-up time of about four years. In that time, there was an average of 6.39 deaths per 1,000 person years in patients with psoriasis on more than 10 percent of their bodies, compared to 3.24 deaths in patients without psoriasis.
Even when researchers adjusted for other demographic factors, patients with a BSA greater than 10 percent were 1.79 times more likely to have died almost double than other people their age and gender who do not have the condition. This risk persisted even when controlling for other risk factors like smoking, obesity, and other major medical conditions.
Severe Psoriasis Predominantly Affects Men
The fact that men are overrepresented in psoriasis registers and consume more psoriasis care have long led researchers to believe that the common skin disease disproportionally affects men. A unique study with 5,438 Swedish psoriasis patients revealed that women have a statistically significant lower incidence of severe psoriasis compared to men.
The study, conducted by researchers at Ume University and Karolinska Institutet, was published in the American Journal of Clinical Dermatology.
"Our results tell us that the well-established gender differences in the utilization of psoriasis care can at least partially be explained by a higher prevalence of more severe disease in men," says Marcus Schmitt-Egenolf, researcher at the Department of Public Health and Clinical Medicine at Ume University and senior author of the study.
The study of gender differences in severe psoriasis cases was based on the Swedish quality register for systemic treatment of psoriasis, PsoReg, which contains detailed disease measurement data on all patients measured with the standard method Psoriasis Area Severity Index (PASI).
In the analysis, the researchers found that women had significantly lower median PASI values than men - 5.4 for women versus 7.3 for men. The findings of more severe psoriasis in men were consistent across all ages and in all areas of the body except for the head. "These findings should motivate a gender perspective in the management of severe psoriasis and its comorbidities, such as cardiovascular and metabolic disease," says Marcus Schmitt-Egenolf.
The researchers point out that the study found no differences between women and men in the use of medications before enrolment in the PsoReg register that may explain the observed sex difference. Instead, the researchers argue, the finding that women have less severe psoriasis can explain the well-known male dominance in systemic treatment of psoriasis.
"For over 70 years, psoriasis researchers have speculated that women have less severe psoriasis compared to men, Schmitt-Egenolf said. Our study is the first to investigate sex differences in psoriasis severity using the golden standard of severity measurement, the PASI score. Furthermore, we have also looked more in-depth at distinct elements of the PASI score. The results allow us to verify this thesis in a nationwide population. However, further research is needed to substantiate our findings in different populations."
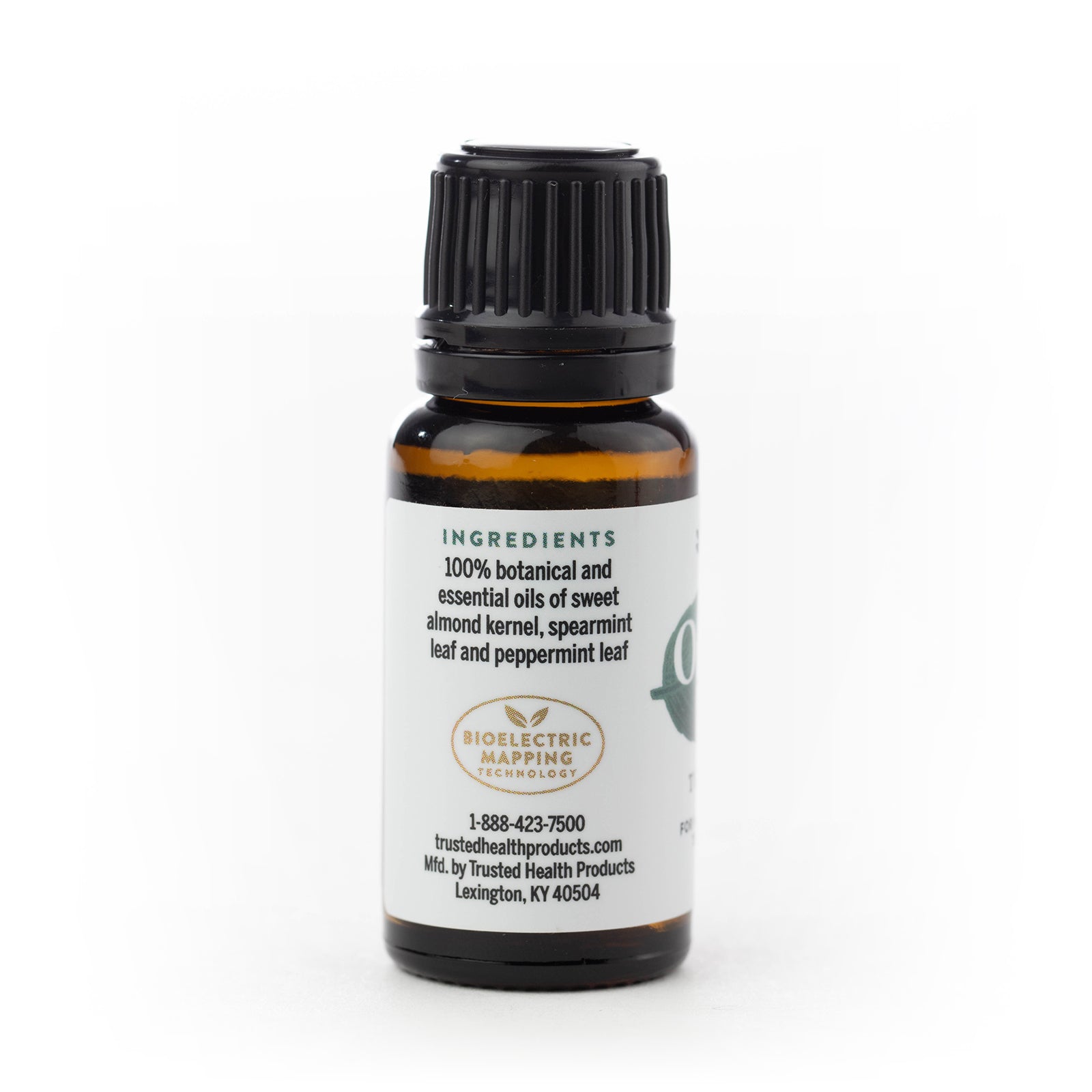
Looking for 100% chemical-free, all-natural nourishing face and body oils? Check out Earth & Elm Nourishing Face Oil and Earth & Elm Nourishing Body Oil. Subscribe to our Trusted Health Club newsletter for more information about natural living tips, natural health, oral care, skincare, body care and foot care. If you are looking for more health resources check out the Trusted Health Resources list.
Reviewed By:
Founder Ray Spotts has a passion for all things natural and has made a life study of nature as it relates to health and well-being. Ray became a forerunner bringing products to market that are extraordinarily effective and free from potentially harmful chemicals and additives. For this reason Ray formed Trusted Health Products, a company you can trust for clean, effective, and healthy products. Ray is an organic gardener, likes fishing, hiking, and teaching and mentoring people to start new businesses. You can get his book for free, “How To Succeed In Business Based On God’s Word,” at www.rayspotts.com.