Melanoma Diagnoses Deserves Second Opinion To Improve Reliability
February 26, 2020
Author: Admin Editor
Tags:
Researchers at UCLA have found that obtaining a second opinion from pathologists who are board certified or have fellowship training in dermatopathology can help improve the accuracy and reliability of diagnosing melanoma. In the study, the value of a second opinion by general pathologists and dermatopathologists were evaluated to see if it helped improve the correct diagnostic classification. To evaluate the impact of obtaining second opinions, the team used samples from the Melanoma Pathology Study, which comprises 240 skin biopsy lesion samples. Among the 187 pathologists who examined the cases, 113 were general pathologists and 74 were dermatopathologists.
The team studied misclassification rates, which is how often the diagnoses of practicing U.S. pathologists disagreed with a consensus reference diagnosis of three pathologists who had extensive experience in evaluating melanocytic lesions. They found that the misclassification of these lesions yielded the lowest rates when first, second and third reviewers were sub-specialty trained dermatopathologists. Misclassification was the highest when reviewers were all general pathologists who lacked the subspecialty training. Second opinions in clinical medicine can increase accuracy, which is a win-win for patients and providers. Better diagnoses lead to better outcomes and efficient use of our healthcare expenditures.
This is definitely something that healthcare providers should consider when faced with these complex and challenging to diagnose skin biopsies. The results show having a second opinion by an expert with subspecialty training provides value in improving the accuracy of the diagnosis, which is imperative to help guide patients to the most effective treatments.
"A diagnosis is the building block on which all other medical treatment is based," says Dr. Joann Elmore, a professor of medicine at the David Geffen School of Medicine at UCLA and researcher at the UCLA Jonsson Comprehensive Cancer Center. "On the other end of these biopsies are real patients: patients answering the late-night, anxiety-inducing phone calls when we inform them of their diagnosis; patients undergoing invasive surgeries; patients weighing their next clinical steps. All patients deserve an accurate diagnosis. Unfortunately the evaluation and diagnosis of skin biopsy specimens is challenging with a lot of variability among physicians. While these findings suggest that second opinions by dermatopathologists improve overall reliability of diagnosis of melanocytic lesions, they do not eliminate or substantially reduce misclassification."
Melanoma Biomarkers Identified
The outlook for patients with advanced melanoma has dramatically improved in recent years because of drugs known as immune checkpoint inhibitors, which mobilize the immune system to attack cancer. These drugs block checkpoint molecules that act as brakes on the immune system. Removing these brakes, checkpoint inhibitors unleash immune defenders such as T cells to recognize and attack cancer.
Scientists at Dana-Farber/Brigham and Women’s Cancer Center recently identified biomarkers in melanoma that could help tailor immunotherapy treatments to maximize the benefits for patients while reducing the likelihood of severe side effects. The findings suggest that the current practice of combining two different types of immune checkpoint blocker drugs in advanced melanoma patients may be the best course in some instances, but not in others, because the immune makeup of some melanoma tumors may cause them to be resistant to one class of checkpoint inhibitors. The study - reported in Science Translational Medicine - revealed that some patients, whose tumors are deficient in a protein needed for the immune system to recognize cancer cells, are unlikely to benefit from ipilimumab, an immunotherapy drug that blocks the CTLA-4 checkpoint, but which has potentially severe side effects. Therefore, identifying such patients with a biomarker test prior to treatment could spare them the adverse effects.
“By looking at how melanoma is avoiding immune detection, we may be able to identify patients who may do just as well with a single agent, with no loss of efficacy, but improved tolerability,” says Scott Rodig, MD, Ph.D., an oncologic pathologist at DF/BWCC and first author on the report. “By contrast, efficacy of anti-PD1 checkpoint blockers like nivolumab depends on “pre-existing interferon-gamma-mediated inflammation within the tumor microenvironment.” Combining the two types of checkpoint blockers “provides a further immune stimulus over individual therapies alone and, in addition, overcomes the limitations of each. Going forward, it would be ideal to have clinical trials in which treatment options are determined in accordance with the results of tissue-based biomarker studies.”
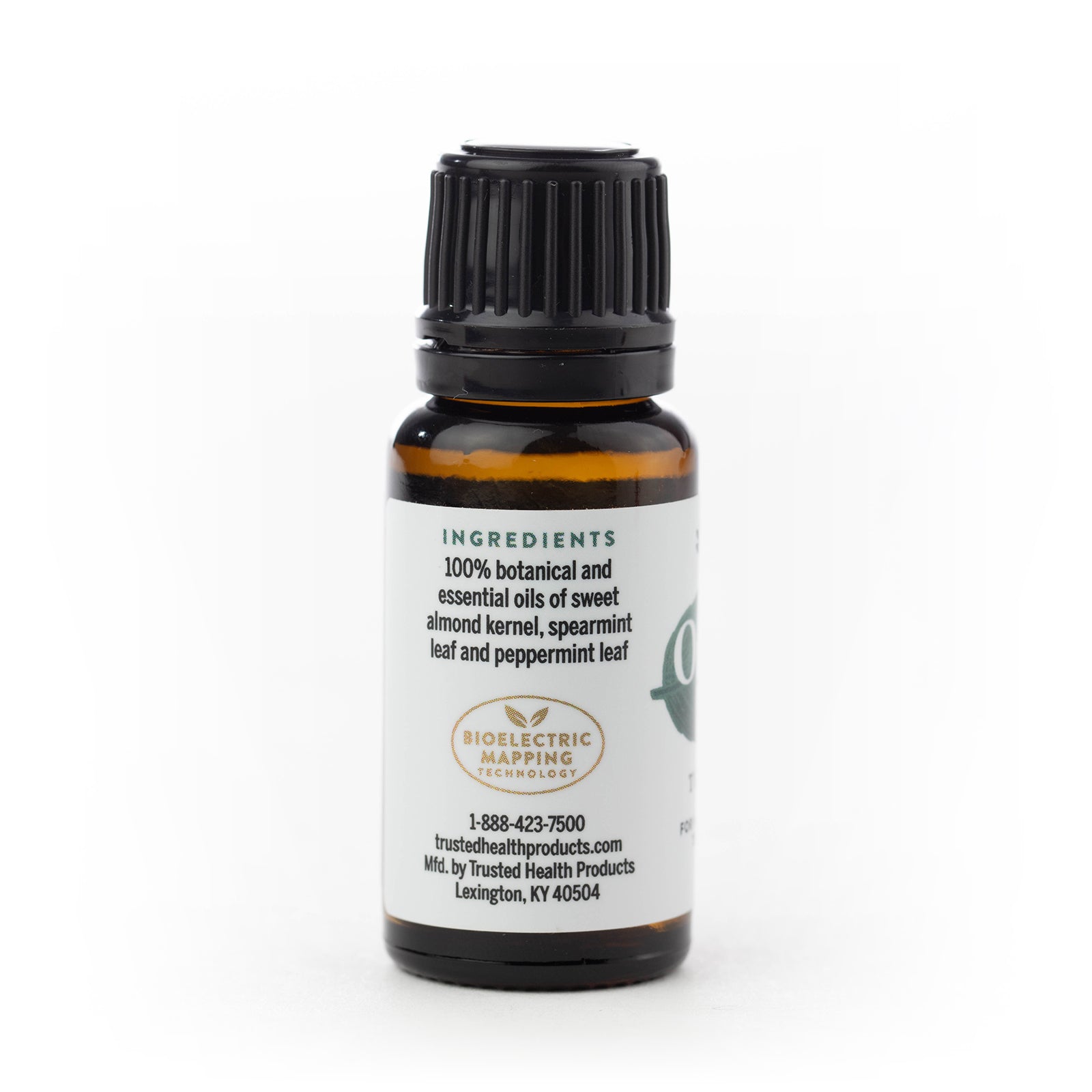
Looking for 100% chemical-free, all-natural nourishing face and body oils? Check out Earth & Elm Nourishing Face Oil and Earth & Elm Nourishing Body Oil. Subscribe to our Trusted Health Club newsletter for more information about natural living tips, natural health, oral health and skincare. If you are looking for more health resources make sure to check out the Trusted Health Resources list.
Written By:
With over 30 years of writing and editing experience for newspapers, magazines and corporate communications, Kevin Kerfoot writes about natural health, nutrition, skincare and oral hygiene for Trusted Health Products’ natural health blog and newsletters.
Reviewed By:
Founder Ray Spotts has a passion for all things natural and has made a life study of nature as it relates to health and well-being. Ray became a forerunner bringing products to market that are extraordinarily effective and free from potentially harmful chemicals and additives. For this reason Ray formed Trusted Health Products, a company you can trust for clean, effective, and healthy products. Ray is an organic gardener, likes fishing, hiking, and teaching and mentoring people to start new businesses. You can get his book for free, “How To Succeed In Business Based On God’s Word,” at www.rayspotts.com.
SHARE
Researchers at UCLA have found that obtaining a second opinion from pathologists who are board certified or have fellowship training in dermatopathology can help improve the accuracy and reliability of diagnosing melanoma.Written By Kevin Kerfoot / Reviewed By Ray Spotts
" aria-label="Share on Pinterest" target="_blank">